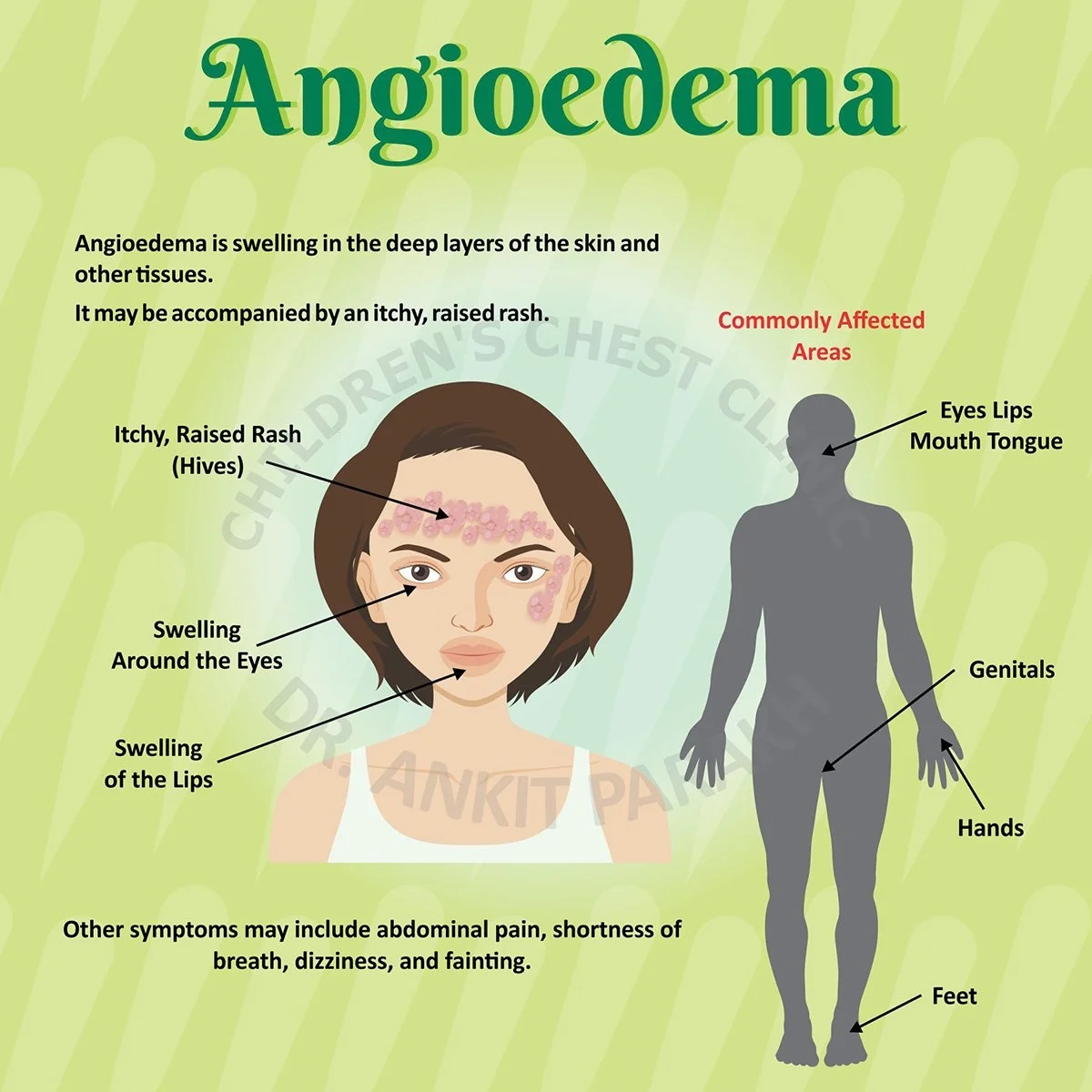
Angioedema is a condition characterized by rapid swelling beneath the skin, often affecting areas such as the face, throat, hands, feet, and sometimes internal organs. For those living with this condition, daily life can be unpredictable and challenging. However, with proper management, awareness, and support, individuals can lead full and active lives.
1. Understand Your Triggers
One of the most critical aspects of living with angioedema is understanding what triggers your episodes. These can vary significantly from person to person and may include:
-
Allergic reactions (food, insect stings, medications)
-
Physical stimuli (pressure, temperature changes, sunlight)
-
Infections (such as colds or sinus infections)
-
Medications like ACE inhibitors
-
Stress and anxiety
Keeping a detailed symptom diary can help you and your healthcare provider identify patterns and potential triggers. The more informed you are, the better equipped you’ll be to prevent flare-ups.
2. Create an Emergency Plan
Angioedema can sometimes lead to severe swelling in the throat, posing a serious risk to breathing. It’s essential to have an emergency plan in place, which includes:
-
Knowing when to seek emergency medical help
-
Carrying an epinephrine auto-injector if prescribed
-
Informing family, friends, and coworkers about your condition and how they can assist
-
Wearing a medical alert bracelet
Having a plan can mean the difference between a manageable situation and a life-threatening emergency.
3. Follow a Treatment Regimen
Treatment for angioedema varies depending on the underlying cause. For instance, hereditary angioedema (HAE) is treated differently than allergic angioedema. Common treatment strategies may include:
-
Antihistamines: Help control allergic-type angioedema.
-
Corticosteroids: Reduce inflammation during a flare.
-
Bradykinin inhibitors or C1-inhibitors: Used for HAE.
-
Avoidance of specific medications that trigger symptoms, like NSAIDs or certain antibiotics.
If a bacterial infection is suspected or confirmed to be a trigger, your doctor might prescribe antibiotics such as cephalexin capsules. Cephalexin is often used to treat skin or respiratory infections, which can sometimes lead to or exacerbate angioedema episodes. Always take medications exactly as prescribed and discuss any side effects or concerns with your healthcare provider.
4. Monitor Medication Side Effects
Some medications can cause or worsen angioedema. ACE inhibitors, for instance, are well-documented triggers. Even seemingly harmless medications, like over-the-counter cold remedies or cephalexin capsules, may contribute to symptoms in sensitive individuals. Always review any new medication with your doctor or pharmacist and report any unusual symptoms immediately.
5. Adopt a Low-Allergen Diet
For those with food-triggered angioedema, identifying and eliminating allergens from your diet is vital. Consider working with an allergist or nutritionist to develop a safe eating plan. Common food triggers include:
-
Shellfish
-
Nuts
-
Eggs
-
Dairy products
-
Food additives or preservatives
An elimination diet, followed by controlled reintroduction, can help identify problematic foods.
6. Strengthen Your Immune System
A healthy immune system can help your body cope better with stressors that might trigger angioedema. Simple lifestyle changes can make a big difference:
-
Eat a balanced diet rich in fruits, vegetables, and whole grains
-
Exercise regularly
-
Get adequate sleep
-
Stay hydrated
-
Manage stress through meditation, yoga, or therapy
In some cases, supplements may be recommended, but always check with your healthcare provider first.
7. Regular Check-ups and Communication
Ongoing communication with your healthcare team is essential. Regular check-ups can help ensure your treatment is still effective and that no new issues have arisen. Keep them updated on:
-
Any new or worsening symptoms
-
Changes in lifestyle or stress levels
-
Effectiveness of your current medications
-
Any reactions to treatments such as cephalexin capsules
This helps your provider make timely adjustments to your care plan.
8. Stay Informed and Advocate for Yourself
Knowledge is power. Educate yourself about the latest research, treatments, and support networks available for angioedema. Join online forums or local support groups to share experiences and gain insight from others who understand your condition.
Advocating for yourself in medical settings is also critical. Many people with rare or misunderstood conditions, like hereditary angioedema, often face misdiagnosis or skepticism. Don’t hesitate to ask questions, request second opinions, or seek specialists when needed.
9. Plan Ahead When Traveling
Traveling with angioedema requires a bit more preparation, but it is entirely doable. Here are a few tips:
-
Carry a detailed list of your medications, allergies, and emergency contacts
-
Pack extra doses of critical medications, including cephalexin capsules if prescribed for an ongoing infection
-
Know the location of nearby hospitals or urgent care centers
-
Carry snacks or meals if you follow a restricted diet
-
Inform travel companions of your condition and how to help in an emergency
10. Emotional and Mental Health Support
Living with a chronic, unpredictable condition like angioedema can take a toll on your mental health. Don’t ignore signs of anxiety, depression, or burnout. Talking to a mental health professional can provide coping strategies and emotional relief.
Additionally, mindfulness practices and support groups can offer a sense of control and community. You’re not alone, and finding others who understand your journey can be incredibly empowering.
Final Thoughts
Angioedema can be unpredictable, but with proactive management, support, and the right medical care, it doesn't have to control your life. From monitoring potential triggers to safely using medications like cephalexin capsules when necessary, these strategies can make living with angioedema more manageable and less stressful.
Stay informed, stay prepared, and prioritize your health both physical and emotional. Your journey with angioedema is unique, but you’re not walking it alone.