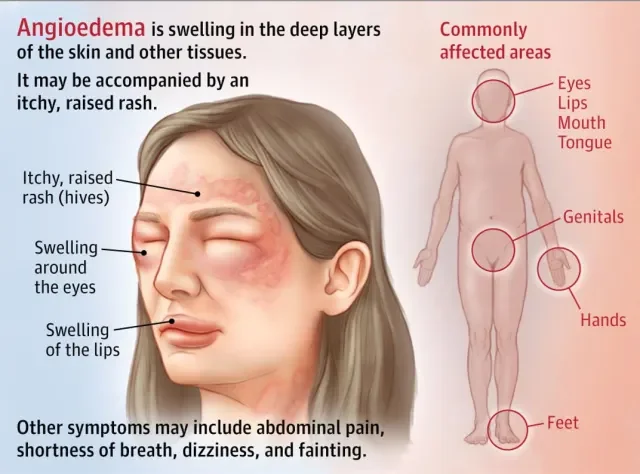
Swelling (edema) in the deeper layers of skin such as the dermis and subcutaneous tissue is a common manifestation of many underlying processes. In some cases, it is benign and self‐limiting; in others, it signals infection, inflammation, vascular or lymphatic dysfunction, or allergic reaction. One classical example is angioedema, which specifically involves swelling of deeper skin layers.
Effective reduction of deeper-layer swelling relies on a multifaceted approach: addressing excess fluid/filtrate, modulating inflammation, supporting tissue drainage, and correcting or treating root causes. Below is a guide to strategies, precautions, and context.
Pathophysiology: Why swelling happens in deeper layers
To tailor therapy, it helps to understand how swelling occurs
Capillary leak / increased permeability
In inflammation or immune activation, capillaries become “leaky,” letting plasma proteins and fluid escape into the interstitial space (dermis + subcutaneous). This increases interstitial pressure and visible swelling.
Hydrostatic / osmotic imbalance
Elevated venous pressure (e.g. in venous insufficiency or heart failure) or low oncotic protein (e.g. hypoalbuminemia) can promote fluid shift into tissues.
Lymphatic drainage impairment
Even a normal leak of fluid is typically cleared by lymphatic vessels; when lymph channels are damaged or blocked (e.g. lymphedema), fluid accumulates.
Allergic / immunologic triggers
In angioedema, mediators (e.g. histamine, bradykinin) cause sudden swelling of deeper tissues (dermis and subcutaneous, sometimes mucosal) without superficial rash.
Infection / cellulitis
Bacterial invasion of deeper skin and soft tissues (cellulitis) causes local inflammatory swelling, redness, heat, and pain. Thus, strategies to reduce swelling must (a) limit fluid influx, (b) enhance fluid egress (venous + lymphatic), (c) suppress inflammation, and (d) treat underlying causatives (e.g. infection, allergy).
Practical Strategies to Reduce Deeper Skin Swelling
Below are evidence-based and empirically supported strategies. Their applicability and safety depend on the clinical scenario, so medical supervision is essential.
1. Elevation & gravity assistance
Elevate the affected limb (or body part) above the level of the heart when possible. This helps reduce hydrostatic pressures and allows passive drainage of fluid.
For facial swelling (e.g. angioedema), gentle head elevation while resting can modestly help.
2. Gentle compression & bandaging
Use compression garments, bandages, or intermittent pneumatic compression devices to provide external pressure that encourages fluid return into the venous and lymphatic channels.
But note: compression must be gentle and well tolerated, especially in inflamed or infected tissue. Improper compression can worsen injury or impair circulation.
3. Manual drainage / massage techniques
Manual lymphatic drainage (MLD) is a specialized soft-tissue massage technique that can be taught by trained therapists to help mobilize lymph fluid from swollen areas toward intact drainage pathways.
For milder swelling, gentle “milking” strokes of soft tissue (towards proximal nodes) may assist fluid shift; avoid harsh pressure over inflamed or tender zones.
4. Cold therapy / cryotherapy
Applying cold compresses (wrapped in soft cloth) for limited intervals (e.g. 10–20 minutes a few times daily) can help constrict capillaries, reduce vascular leakage, and provide symptomatic relief.
However, avoid overuse of cold in areas with compromised circulation or neuropathy.
5. Pharmacologic modulation of inflammation
Nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce inflammatory mediator release, capillary permeability, and swelling, when not contraindicated.
Corticosteroids (systemic or local) may be used in selected inflammatory or allergic etiologies (e.g. angioedema) under physician direction.
In allergic angioedema, antihistamines and sometimes epinephrine (in acute severe cases) are standard.
6. Fluid management and diet
Salt (sodium) restriction: since sodium draws water, lowering salt intake helps reduce fluid retention. This is especially relevant in systemic edema.
Adequate hydration: paradoxically, in many cases, maintaining good hydration helps the body regulate fluid balance effectively and reduces edematous retention due to “conserving” mechanisms.
Monitor and manage underlying systemic conditions (e.g. heart failure, kidney disease) that may drive generalized edema.
7. Physical activity / movement
Gentle movement, walking, or muscle contractions in the affected area help promote lymphatic and venous return via the “muscle pump” mechanism.
Avoid prolonged immobility or being sedentary in one posture for long periods (standing or sitting), which worsens pooling.
8. Skin care and protection
Keep skin clean, moisturized, and intact, especially over swollen zones. Cracks or breaks allow bacterial entry and increased inflammation.
Avoid heat, harsh irritants, and trauma in the area.
Use gentle cleansers, mild soaps, and emollients (moisturizers) to maintain barrier integrity.
9. Monitor & treat infection
In any swollen area that is red, warm, or tender (or with systemic signs like fever), suspect cellulitis or soft tissue infection. In such cases, antibiotic therapy is mandatory.
In bacterial soft tissue infection, prompt systemic antibiotics help reduce the infection and thereby alleviate the swelling secondary to inflammation.
Special Considerations: Angioedema and Deep Skin Swelling
Since angioedema is a classical instance of swelling in deeper skin layers, some points deserve highlighting:
Angioedema is typically mediated by histamine or bradykinin, depends on underlying cause (allergic, hereditary, drug induced).
It can progress quickly and threaten the airway if it involves facial or throat tissues; urgent medical care is required.
Supportive measures (elevation, cold compresses, avoidance of triggers) help, but medical therapy (e.g. antihistamines, steroids, epinephrine) are standard in acute management.
Preventive therapy may be needed in recurrent angioedema (e.g. for hereditary forms), but that is beyond scope of a general guide.
Limitations, Risks & Warnings
Always verify circulatory sufficiency before applying compression; in ischemic limbs, compression may harm.
Cold therapy in neuropathic or vascularly compromised tissue must be used cautiously.
NSAIDs and steroids have side effects (renal, GI, immunosuppression).
In swelling that doesn’t respond or recurs, deeper pathology (e.g. venous insufficiency, lymphatic obstruction, kidney/heart disease) must be investigated.
Do not self-treat severe or rapidly progressing angioedema or cellulitis at home seek medical attention.
Example / Case Illustration (Hypothetical)
Consider a patient with swelling of the lower leg (subcutaneous edema) after a minor skin fissure that got infected:
On exam: swelling, erythema, tenderness → suspected cellulitis.
Start systemic antibiotics → reduction in infection load, inflammatory mediator release decreases.
Simultaneously: leg elevated, compression bandage applied, patient gently moves foot/ankle.
Manual lymph drainage by a therapist, salt intake restricted.
Skin kept clean, moisturized; passively monitor for worsening signs.
Over days, swelling recedes as inflammatory leakage subsides and drainage is effective.
If swelling had been exclusively from heart failure, antibiotics wouldn’t help; the emphasis would shift to diuretics, cardiac therapy, compression, salt restriction, and drainage support.
Commercial / Distribution Note: Cephalexin Capsules Distributors
As requested, here’s a brief note incorporating the keyword cephalexin capsules distributors:
In the context of managing infections (such as cellulitis), systemic antibiotics like cephalexin are frequently prescribed. Cephalexin (a first-generation cephalosporin) is distributed globally by pharmaceutical companies and wholesalers. For instance, Aurobindo Pharma markets Cephalexin Capsules 250 mg in the U.S. market.
In India, many pharmaceutical distributors and wholesalers supply cephalexin capsules to pharmacies and hospitals. The cephalexin API (active pharmaceutical ingredient) is also traded by wholesale firms (e.g. Silveron Industries offers cephalexin API) which are upstream to capsule manufacturing and distribution.